About São Paulo State University
São Paulo State University
Articles by São Paulo State University
The lifestyle modification effectiveness in reducing Hypertension in a Brazilian Community: From the epigenetic basis of Ancestral Survival to the Contemporary Lifestyle and Public Health Initiatives
Published on: 12th May, 2017
OCLC Number/Unique Identifier: 7317592099
High blood pressure (HBP) is a strong, independent and etiologically relevant risk factor for cardiovascular and therefore, the leading cause of preventable deaths worldwide. Hypertension has high medical and social costs. Due to its many associated complications, the use of medical services create high costs with medications which represent almost half of the estimated direct expenses. Free distribution of more than 15 medications for HyPERtension and DIAbetes (HIPERDIA program) clearly shows the important role of drugs in the Brazilian Government’s effort to tackle these two diseases. Notwithstanding, the prevalence of HBP is rising in parallel with other NCDs. It is known that HBP results from environmental and genetic factors, and interactions among them. Our ancestors were often faced with survival stresses, including famine, water and sodium deprivation. As results of natural selection, the survival pressures drove our evolution to shape a thrifty genotype, which favored/promoted energy-saving and sodium/water preservation. However, with the switch to a sodium- and energy-rich diets and sedentary lifestyle, the thrifty genotype and ancient frugal alleles, are no longer advantageous, and may be maladaptive to disease phenotype, resulting in hypertension, obesity and insulin resistance syndrome. Low-grade chronic inflammation and oxidative stress would be the underlying mechanisms for these diseases. HBP is often associated with unhealthy lifestyles such as consumption of high fat and/or high-salt diets and physical inactivity. Therefore, alternatively to medicine drugs, lifestyle and behavioral modifications are stressed for the prevention, treatment, and control of hypertension. A lifestyle modification program (LSM) involving dietary counseling and regularly supervised physical activity (“Move for Health”) has been used for decades, in our group, for NCDs primary care. Retrospective (2006-2016) data from 1317 subjects have shown the top quartile of blood pressure(142.2/88.5mmHg) differing from the lower quartile (120.6/69.2mmHg) by being older, with lower schooling, lower income and, lower physical activity and aerobic capacity. Additionally, the P75 showed higher intake of CHO, saturated fat and sodium along with lower-diet quality score with a more processed foods. They showed higher body fatness and prevalence of metabolic syndrome along with higher pro-inflammatory and peroxidative activities and insulin resistance. In this free-demand sample, the HBP rate was 51.2% for SBP and 42.7% for DBP. The rate of undiagnosed HBP was 9.8% and only 1/3 of medicated patients were controlled for HBP. After 10 weeks of LSM the HBP normalization achieved 17.8% for SBP and 9.3% for DBP with a net effectiveness of 8.5% and 2.4%, respectively. The reduction of HBP by LSM was followed by increased aerobic conditioning and reduced intake of processed foods along with decreased values of BMI, abdominal fatness, insulin resistance, pro-inflammatory and peroxydative activities. Importantly, once applied nationwide this LSM would save HBP medication for 3.1 million of hypertensives at an economic saving costs of US$ 1.47 billion a year!
Treating Blood Hypertension in a Brazilian Community: Moving from Reactive Homeostatic Model to Proactive Allostatic Healthcare
Published on: 26th January, 2018
OCLC Number/Unique Identifier: 7338864811
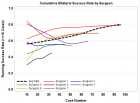
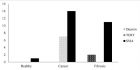
The responsiveness of hypertensive subjects to different types of physical exercises and length of intervention, has been investigated in samples of our dynamic cohort study (“Move for Health” program) based on spontaneous demand for healthy lifestyle with supervised exercises and dietary counseling. After clinical selection and baseline assessments they were spontaneously assigned to exercise protocols of strength (PAc) isolated or combined with endurance (walking) exercises (PMi) daily or in alternated days(PMiA), hydrogymnastics(PHy) and tread mill high- intensity exercises(PHit), applied during 10(experiment 1) and 20(experiment 2) weeks of intervention. Baseline demographic, socioeconomic, anthropometric and physical activity and fitness characteristics were similar among protocols. Ten-week training improved VO2max. Similarly in all protocols while hand grip increased only in PAc. In average, there was a 16% reduction rate of hypertension rate from baseline with both, SBP and DBP, reduced by PHy and only SBP by the PMi. After adjustments hypertension was more reduced by PAc, PMi and PHy. In the 20-week experiment, higher SBP was similarly reduced by PAc or PMiA and DBP by PMiA, after adjustments. Hence, so far, our generated data suggest physical exercises as an effective tool for hypertension reduction, from 10 weeks to 3 year-long supervised protocols composed by surface or aquatic activities with strength or endurance exercises. PAc takes longer and short-period responsiveness can be achieved by either combined (strength-endurance) or hydrogymnastic exercises. Thus, exercise training is a time-and type-dependent tool, feasible, costless and scientific-based rheostatic-allostatic alternative for the current “sick-care” drug-dependent homeostatic approach to hypertension med care.
Hospital hyperglycemia protocol for non-critical patients in a tertiary-level university hospital
Published on: 26th October, 2022
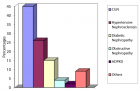
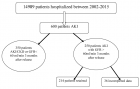
Diabetes Mellitus (DM) is a frequent comorbidity in hospitalized patients, with prevalence ranging from 15% - 35%. However, in almost half of the cases, this antecedent is omitted in the medical records or even unknown by the patient. Furthermore, about 10% of hospitalized individuals may have hyperglycemia of stress, a condition characterized by transient and reversible elevation of blood glucose, in the presence of acute circumstances, such as trauma, surgery, medications, shock, or infections [1].

HSPI: We're glad you're here. Please click "create a new Query" if you are a new visitor to our website and need further information from us.
If you are already a member of our network and need to keep track of any developments regarding a question you have already submitted, click "take me to my Query."